What is adrenal insufficiency?
In people with normal adrenal function, the adrenal glands produce a number of hormones that rise and fall naturally throughout the day, and in response to stress and illness.
Adrenal insufficiency is a condition where the adrenal glands cannot produce enough adrenal corticosteroid hormones. This can be due to a problem with the adrenal glands (called primary adrenal insufficiency) or the pituitary gland (called secondary adrenal insufficiency).
Primary adrenal insufficiency is a rare condition also known as Addison’s disease. This affects around 2,500 Australians, with 100 new diagnoses made each year 1. In primary adrenal insufficiency, the levels of all corticosteroid hormones are affected.
Secondary adrenal insufficiency is more common than primary adrenal insufficiency. This occurs when the pituitary gland cannot produce enough of the hormone adrenocorticotropic hormone (ACTH) to signal to the adrenal glands to make adrenal corticosteroid hormones. In secondary adrenal insufficiency, the salt-retaining hormone aldosterone is not affected.
What causes adrenal insufficiency?
Primary adrenal insufficiency
Most cases of primary adrenal insufficiency are due to an autoimmune disorder, where the immune system attacks and destroys the outer part of the adrenal gland (the adrenal cortex). Other causes include:
- Congenital adrenal hypoplasia
- Severe bacterial or fungal infections – e.g. tuberculosis
- Haemorrhage (bleeding) in the adrenal gland
- Removal of both adrenal glands (adrenalectomy)
- Cancers, such as lymphoma, or solid tumours (usually spread from other sites) affecting both adrenals
- Medications for tumours of the adrenal gland
- Genetic causes (rare)
Secondary adrenal insufficiency
Causes of secondary adrenal insufficiency include:
- Congenital hypopituitarism
- Tumour (or cysts) in and around the pituitary gland
- Surgery or radiation to treat tumours in the pituitary region
- High doses of glucocorticoid medications used to treat some conditions e.g. for asthma, rheumatoid arthritis
- Trauma – head injury
- Some rare inflammatory diseases affecting the pituitary or hypothalamus.
Congenital adrenal hyperplasia (CAH)
A group of rare inherited conditions, present at birth, which usually result in high levels of adrenal androgens, low cortisol and variable mineralocorticoid levels. People with CAH share features with primary adrenal insufficiency and some are at risk of adrenal crisis.
Symptoms of adrenal insufficiency
Many symptoms of adrenal insufficiency are not-specific to this condition, and therefore can be hard to identify. The symptoms can also develop very slowly, and are often only identified when there is a sudden worsening of symptoms, called an adrenal crisis.
Symptoms of primary and secondary adrenal insufficiency include:
Specific symptoms associated with primary adrenal insufficiency include:
How is adrenal insufficiency diagnosed?
1. Medical history
Your doctor will ask you questions about your health, symptoms and medical history, including if you take any medications or use supplements, have other health conditions, your family history.
2. Blood tests
Your doctor will check the level of cortisol in your blood to determine whether you may have adrenal insufficiency. This blood test generally needs to be performed in the morning (before 9am) as cortisol levels naturally fall over the day. This involves taking a small amount of blood and sending it to a laboratory for testing. At the same time, your doctor may request additional measurements from the blood sample. These can include ACTH, renin, aldosterone, glucose, sodium and potassium. If secondary adrenal insufficiency is suspected, other pituitary gland hormones will be measured.
Different laboratories use different methods for testing, and so normal reference ranges can vary. This can make comparison of results between laboratories and other people difficult.
3. Corticotropin Stimulation test (Short Synacthen test)
This test is used to establish adrenal insufficiency. It involves injecting Synacthen, a shortened synthetic form of ACTH, which stimulates the adrenal glands to make cortisol. Before the test, a blood sample is taken to measure baseline cortisol and ACTH. The Synacthen is then injected into a muscle or vein, and further blood samples are collected 30 and/or 60 minutes later to again measure cortisol. This test can be done at any time of the day, but commonly in the morning.
4. Blood test to investigate the cause of adrenal insufficiency
It is important to investigate the cause of adrenal insufficiency, so that the right treatment can be given. This can include another blood test to check for specific antibodies for autoimmune disease or to identify genetic causes.
5. Computer tomography (CT) scan
If you have primary adrenal insufficiency, your doctor may want to look at the size and shape of your adrenal glands. This is usually done using an imaging method called computerised tomography (CT scan), and occasionally with a MRI scan (see below). A CT scan uses X-ray and computer technology to create pictures of the body. These pictures can help identify whether the adrenal glands are enlarged, which may suggest the presence of an infection (e.g. tuberculosis) or a genetic condition. It can also be used to check for tumours.
6. MRI scan
If you have secondary adrenal insufficiency, your doctor may check the size and shape of your pituitary gland. This is usually done using a scan called magnetic resonance imaging (MRI). A MRI scan uses a magnetic field and radio waves to take pictures of parts of the body. These pictures can help assess the structure of the pituitary gland, and to check for pituitary tumours.
How is adrenal insufficiency treated?
The treatment of adrenal insufficiency will be customised to your needs. Your doctor will discuss with you the type of adrenal insufficiency and which hormones are affected. The goal of treatment is to replace the missing hormones and improve symptoms. For most people, this usually means ongoing treatment. It is quite common for doses to be adjusted frequently at the start of treatment.
Glucocorticoid replacement therapy
This is used to treat both primary and secondary adrenal insufficiency.
Because people with adrenal insufficiency have inadequate levels of the hormone cortisol, this therapy is designed to give back (or replace) this missing hormone. The doses administered aim to replicate the expected normal range of cortisol – that is, the doses are the same as those found in people without adrenal insufficiency. The main types of glucocorticoid replacement therapies in Australia are hydrocortisone (typically 15-25mg daily) and cortisone acetate (typically 20-30mg daily). These are oral medications (tablets) taken 2 or 3 times per day. Your doctor will discuss how many doses you will need. The highest daily dose is taken soon after waking in the morning, when natural cortisol levels are at their highest. If two daily doses are prescribed, the second dose will generally be taken early in the afternoon. If three daily doses are prescribed, the second will be taken at lunch and the third in the later afternoon.
Another glucocorticoid medication is prednisolone (usually 3-6 mg daily), which also acts like cortisol. This medication is often only needed once per day, as it is active for a longer period. While once a day dosing is more convenient, people treated with prednisolone are more likely to receive slightly more glucocorticoid than they need, which can lead to side effects.
Glucocorticoid replacement medication should not be ceased abruptly.
Mineralocorticoid replacement therapy
This therapy is needed only for treatment of primary adrenal insufficiency where aldosterone levels are low.
In Australia, mineralocorticoid replacement medication is with fludrocortisone (usually 0.05-0.3mg daily), which is taken as a tablet. It is taken every day in the morning. There is no need for salt to be reduced in the diet while on this medication. Fludrocortisone does not have to be increased during illness.
Check-ups with your doctor at least once a year will help to make sure you are getting the right amount of fludrocortisone to minimise your symptoms. At these check-ups, your doctor may check your blood pressure while sitting and standing, ask you whether you feel light-headed or dizzy when you stand up, ask about salt cravings, measure the levels of salts (sodium and potassium) in your blood and assess any swelling (e.g. around the ankles).
Androgen (DHEA) replacement therapy
This therapy is not routinely used, as it is not generally effective. Perhaps a small group of patients with adrenal insufficiency may experience some benefit. It is sometimes used where symptoms, such as low libido (sex drive), anxiety, depressive symptoms or low energy levels, still occur despite other hormone replacement being adjusted to optimal levels. There is no long-term information to indicate that DHEA is safe.
DHEA is taken orally in the morning. Your doctor may recommend trialling this treatment for 6 months to see if it improves symptoms. DHEA can have side effects in some people, such as acne, changes to menstrual cycle, increased facial hair and a deepened voice, if given in excessive doses. In Australia, there is not a pharmaceutical preparation approved by the Therapeutic Goods Administration so it is often sourced from compounding pharmacies. It comes as a capsule or troche (wafer).
DHEA should not be used if you are pregnant or breastfeeding, or have breast cancer, uterine cancer, ovarian cancer, endometriosis or PCOS.
Adjusting treatment during illness, surgery, trauma or stress
In people with adrenal insufficiency, cortisol levels do not automatically rise in response to illness, surgery, trauma or stress, as the adrenal glands cannot produce enough cortisol. This is why it is essential to increase glucocorticoid doses at these times to avoid an adrenal crisis.
An increase in the dose of glucocorticoid is needed if you have:
- Illness with fever – double for milder illness and triple for more severe illness for 3 days or until well.
- Surgery or childbirth – require additional glucocorticoid doses, and this should be planned ahead of time.
- Severe trauma (e.g. a car accident or sports injury)
- High amounts of stress
Your doctor will discuss this with you and advise when and how to adjust your medications. This sick day management plan can be downloaded and completed by your doctor. This provides a clear outline for how much medication to take when you are not well.
When diarrhoea or vomiting occurs, it is unlikely the medication is being absorbed properly. If these occur, the medication needs to be given by injection.
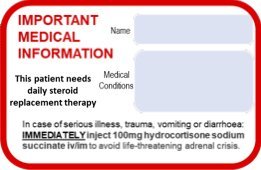
Injectable hydrocortisone (100mg; Solu-Cortef) can be given intramuscularly (into a muscle) or subcutaneously (under the skin) by patients or their family for times when oral medication is not enough or possible, such as vomiting, diarrhoea, other serious illness or if unconscious. Ask for training in this if it is not offered promptly after your diagnosis. Instructions about how to administer Solu-Cortef should also be carried, in case you are unconscious.
After Solu-Cortef is administered, you should still be transported to medical care (emergency department or hospital).
What is an adrenal crisis?
An adrenal crisis can occur when a person with adrenal insufficiency is exposed to severe physical or psychological stress, such as infection, illness, surgery or trauma, and experiences low levels of cortisol. This is a medical emergency.
Symptoms of an adrenal crisis
The symptoms of an adrenal crisis include:
- Severe low blood pressure (shock)
- Altered level of consciousness and/or confusion
- Worsening of all symptoms of adrenal insufficiency and sometimes sudden pain in the back, stomach or legs
Treatment during an adrenal crisis
In cases of adrenal crisis, use the injectable hydrocortisone (Solu-Cortef) as advised above, BEFORE professional help (paramedics, doctors) arrives. This is very important even if going to hospital, as there can be delays in processing Emergency Department patients. After Solu-Cortef is administered, you should still be transported to medical care (emergency department or hospital).
How can I be prepared?
If you are taking cortisol replacement / steroid therapy, know your sick day management plan and wear an alert bracelet and carry a steroid card
Your doctor will go over your sick day management plan with you. This will include when and how to adjust your medication when you are not well. You can download and complete this sick day management plan with your doctor so you have a record. It is a good idea to take a photo of this on your phone, so that it can be with you at all times.
It is advisable to wear a medical alert bracelet with information, such as “give hydrocortisone” to inform medical attendants that you need medication if you are too unwell to tell them in person. It is also useful to tell your friends and family about your need for extra medication when you are unwell.
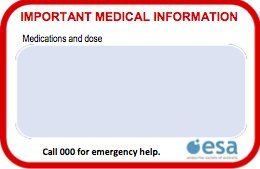
You should also carry emergency medical information with you, such as your medications and the name of your doctor.
A “Steroid card” for your wallet or purse is also recommended. This card can be used to record the details of your medical condition and medications for use in emergency situations.
The ESA credit-card sized steroid card is available for download here.
Your doctor can help you fill in the card. This can then be folded in half and laminated to fit easily in your wallet, purse or bag.
By carrying emergency medical information, others can help if an adrenal crisis occurs.
Have regular check-ups with your doctor
Check-ups with your doctor at least once a year will help to make sure you are taking the right dose of medication to minimise your symptoms. At these check-ups, your doctor may check your weight, blood pressure, energy levels and if you have any swelling, and may assess your bone health.
FAQs about adrenal insufficiency
When to see your doctor
If you have symptoms suggesting adrenal insufficiency, you should see your doctor. Your doctor can conduct tests to identify the cause of your symptoms and start you on any medications you may need.
If you are having signs of adrenal crisis, it is important to get medical help quickly, using emergency services (dialling 000) if needed.
Questions to ask your doctor
Seeing your doctor or having a medical problem can be stressful. It often takes time for information to sink in and it is very common to feel overwhelmed by what is happening.
Sometimes it helps to write down questions before you go.
Some medications can interfere with glucocorticoid and/or mineralocorticoid therapy. This can mean that increased replacement doses are needed. If you are given any new medications, it is advisable to ask your doctor if they will interfere with your glucocorticoid therapy.
Some other questions that might be useful for you are:
- What type of adrenal insufficiency do I have?
- Is my adrenal insufficiency permanent or temporary?
- Will I need to take hormone replacement medication?
- How often do I need to take my medication?
- When should I change the dose of my medication?
- Does my medication have any side effects?
- Do I need to wear a medical alert bracelet?
- Do I need a steroid card for my wallet?
- Do my other medications interfere with my adrenal insufficiency medications?
- Do I need a CT or MRI scan?
- Do I need another appointment?
Common terms and definitions
Adenoma – a non-cancerous tumour that occurs in glands
Adrenal – gland that sits above each kidney. It is divided into an outer layer (cortex) that makes corticosteroids and an inner layer (medulla) that makes adrenaline
Adrenalectomy – the surgical removal of one or both adrenal glands
Adrenal androgens – sex hormones made by the adrenal gland
Autoimmune disorder – a condition where the body’s immune system attacks healthy cells
Benign – a benign tumour is one that is not cancerous
Carcinoma – a type of cancer
Congenital adrenal hyperplasia (CAH) – is a genetic condition that causes a block in the production of adrenal hormones, leading to enlargement of the adrenal glands
Congenital adrenal hypoplasia – a genetic condition that results in failure of the adrenal gland to develop and make enough adrenal hormones
Congenital – a condition present from birth
Corticosteroid – type of steroid hormone made by the adrenal gland, OR related medication. This includes glucocorticoids (cortisol), mineralocorticoids (aldosterone) and adrenal androgens (DHEA)
Cyst – an enclosed pocket of fluid in the body
Glucocorticoid – the natural adrenal hormone cortisol; medication such as hydrocortisone, cortisone acetate, prednisolone and dexamethasone
Hypopituitarism – a condition where the pituitary gland cannot produce enough pituitary hormones
Insomnia – trouble sleeping or staying asleep
Hypothalamus – area in the base of the brain that controls the output of pituitary gland hormones
Malignant – Contains cancerous cells
Mineralocorticoid – the natural salt preserving hormone aldosterone; medication – fludrocortisone
Pituitary – small gland situated just underneath the brain that controls hormone production from a number of other glands such as the thyroid, adrenals, ovaries and testes
Synacthen – synthetic ACTH, used to test for adrenal insufficiency
Tumour – an abnormal swelling or growth in the body. Can be benign or malignant
The content on this page was medically reviewed:
A/Prof Warrick Inder, Prof Peter Fuller, A/Prof David Henley, Prof David Torpy
We are extremely grateful to Grahame Collier and Tammy McLandsborough from The Australian Addison’s Disease Association Inc, and Dr Yi Yuen Wang and volunteers from the Australian Pituitary Foundation, for reviewing this information.
Page last reviewed on 11 Sep 2023