What is Cushing’s Disease?
Cushing’s disease is a condition that occurs when a tumour in the pituitary gland causes the body to produce too much of the hormone cortisol.
The pituitary gland is located at the base of the brain and produces a number of hormones that control various systems of the body. One of these hormones is adrenocorticotrophic hormone (ACTH). When released, ACTH travels in the blood stream and acts as a messenger, signalling the adrenal glands (located in the abdomen) to produce cortisol.
In Cushing’s disease, a tumour located in the pituitary gland produces excess amounts of ACTH. This, in turn, stimulates the adrenal glands to produce too much cortisol.
Cushing’s syndrome is a term that describes a pattern of symptoms caused by too much cortisol in the body. The excess cortisol may be a result of Cushing’s disease (specifically referring to a pituitary tumour) or be caused by other circumstances that might cause high cortisol levels, including long term use of corticosteroid medications, excessive alcohol consumption, severe depression or an adrenal or lung tumour.
What causes Cushing’s Disease?
Cushing’s disease is most often caused by a small benign (non-cancerous) tumour of the pituitary gland that produces too much ACTH.
Symptoms of Cushing’s Disease
Many symptoms and signs of Cushing’s syndrome are common in other conditions and are not specific to Cushing’s disease. They also can develop over a long period of time, making Cushing’s syndrome hard to identify.
Physical symptoms can include:
Other symptoms may include:
How is Cushing’s Disease diagnosed?
Diagnosing Cushing’s disease can be difficult. Not only are many of the symptoms common in other conditions but tumours in the pituitary causing Cushing’s disease are typically small. Furthermore, symptoms can also progress very slowly, making changes difficult to notice by patients and family.
No single test can be used to diagnose Cushing’s disease. A number of tests are needed, firstly to confirm that your cortisol levels are high (points 3-5 below), and then to identify the cause as originating from the pituitary or not (points 6-9 below). Sometimes additional tests may be needed to screen for other health conditions commonly occur with Cushing’s disease (points 10-11 below).
1. Medical History and Physical Examination
Your doctor will ask you questions about your health, symptoms and medical history, including if you take any medications or use supplements, have other health conditions and your family history. Examination is important to measure your weight, blood pressure and identify signs that might support a diagnosis of Cushing’s syndrome.
2. Blood tests
A blood test will be used to measure the levels of cortisol and ACTH in your blood. This blood test generally needs to be performed in the morning (before 9am) as in normal circumstances cortisol levels fall over the day. You may be asked to fast the night before. A small amount of blood is taken and sent to a laboratory for testing. The doctor may also be interested in measuring the levels of other pituitary hormones as well.
3. 24-hour urinary free cortisol test
This test measures the level of cortisol produced by your body over one full day. You will be provided with a urine collection jug and a larger container to collect all urine passed over a 24-hour period (1 full day). For the test, it is important to choose a day where you will be able to collect all your urine across the whole time. This is because an incomplete collection will make the test invalid, and the whole process will need to be repeated on another day.
The 24-hour period starts immediately after the first urination in the morning and continues until the same time the following day. Collect all urine in the collection jug and then add to the larger container, which should be kept refrigerated until taken back to the pathology centre. It is important not to drink excess fluids over the 24 hours of the collection as large urine volumes also make the test unreliable.
4. Late night salivary cortisol test
In healthy people, cortisol levels rise in the morning and fall across the day, with the lowest levels seen late at night. In people with Cushing’s disease, this daily rhythm can be lost. Measuring cortisol levels late at night checks whether cortisol levels decrease through the night.
This test can be done at home. It involves taking a swab/sample of your saliva at midnight. It is important not to eat, drink, smoke or brush your teeth for 30 minutes before collecting the sample. For the collection, you should leave the swab in your mouth for 2 minutes or until it is soaked in saliva. To ensure accurate results, do not chew the swab or touch it with your hands.
5. Low dose dexamethasone suppression test
Dexamethasone is a medication that usually reduces cortisol levels in healthy people. Your doctor may organise this test to check whether your body can reduce cortisol production in response to this medication. This test is usually done overnight, but may also be done over 2 days. Sometimes the test needs to be done on a couple of occasions at different dexamethasone doses.
For the overnight low dose dexamethasone suppression test, 1mg of dexamethasone (in tablet form) is taken at home at around 11pm. The following morning at exactly 8am (9 hours after swallowing the dexamethasone), a blood sample will be taken to measure cortisol levels. You will need to attend a pathology centre or a medical clinic for this blood test, and it is a good idea to book in with the pathology lab for this test as the timing is very important.
For the two-day low dose dexamethasone test, a morning blood sample is taken to measure baseline cortisol and ACTH levels. A 0.5mg dexamethasone tablet is then taken exactly every 6 hours over the next 2 days. This includes late at night and early morning. After the two days, you will have another morning blood test to again measure cortisol and ACTH levels.
6. High-dose dexamethasone suppression test
High doses of dexamethasone usually suppress cortisol if the tumour producing the excess ACTH is located in the pituitary gland, but not if the tumour is located in other organs of the body.
This test can be done in three ways: dexamethasone can be given in tablet form as a single dose (oral) or given intravenously (into the vein). Less commonly, the dexamethasone is taken as a tablet over two days.
For the oral overnight dexamethasone suppression test, an 8mg dexamethasone dose is taken at home at around 11pm. A blood sample is then taken at a pathology centre at exactly 8:00am the following morning, to check cortisol levels.
The intravenous high dose dexamethasone suppression test is performed at a specialised endocrine testing centre as a day patient following an overnight fasting period. A high dose of dexamethasone will be administered through a cannula placed in a vein in the arm over a period of five hours. A blood sample will be collected through a cannula in the other arm every 30 minutes to measure your ACTH and cortisol levels.
The oral two-day high dose dexamethasone suppression test begins with a morning blood sample taken to measure cortisol and ACTH. A 2mg dose of dexamethasone is then taken exactly every 6 hours over the next 2 days. This includes late at night and early morning. After the two days, you will have another morning blood test to again measure cortisol and ACTH levels.
7. CRH test
The corticotropin releasing hormone (CRH) test is sometimes used to help determine the source of high cortisol and ACTH levels.
In healthy people, ACTH production increases in response to a hormone called corticotropin releasing hormone (CRH). If the tumour causing excess ACTH is located in the pituitary gland, then ACTH levels will increase in response to CRH, whereas tumours outside of the pituitary usually don’t respond to CRH.
Before the test, you will have a cannula (thin tube) placed in a vein in your arm. This will be used to take blood samples and administer the CRH, avoiding the need for repeat needles.
Blood will be collected through the cannula to measure baseline ACTH and cortisol levels. CRH will then be administered through the cannula. Blood samples will then be collected every 15 minutes for up to 90 minutes to assess cortisol and ACTH.
8. MRI scan
If the previous tests have confirmed Cushing’s syndrome (high cortisol levels) and suggest this is due to a pituitary tumour (Cushing’s disease), your doctor will send you for an MRI scan of the pituitary. Knowing the size and location of a tumour is important for planning treatment.
An MRI scan uses a magnetic field and radio waves to take pictures of parts of the body. Before having an MRI, you will usually change into a gown and remove any watches or other metallic objects. You might be given earplugs or headphones, as the MRI machine can be noisy. Some people with metal in their body (for example, some pacemakers, welding injuries with metallic foreign bodies in their eyes) cannot have an MRI.
Before the scan, the staff will put a cannula in a vein in your arm or hand so they can inject a contrast solution later during the scan. This dye helps to see the outline of the tumour against the normal pituitary tissue.
For the scan, you will lie on a platform that slides into the MRI machine. You will need to lie very still while inside the machine, as movement can blur the images. When inside the MRI machine, you will still be able to talk to the operator through an intercom system. The scan can take up to an hour.
After the initial scans, you will be moved out of the tunnel a little, so the contrast dye can be injected into the cannula in your hand/arm for a second set of scans. You may feel cold in your arm as the dye is injected. After the scan, you will be moved completely out of the tunnel. The cannula will then be removed, and the site bandaged.
9. Inferior petrosal sinus sampling (IPSS)
This test checks whether the ACTH-producing tumour is in the pituitary gland. While this test may be done when the results of other tests are inconclusive, it can also be done when a small pituitary tumour is observed on MRI. This is because in the general population pituitary tumours that are non-functioning (i.e. not causing excess hormone production) are very common, and doctors don’t want to assume the tumour is the cause of the ACTH secretion.
The IPSS test measures ACTH in the veins that drain blood directly from the pituitary gland. These veins are called the inferior petrosal sinuses.
Before your test: The night before you go to hospital for this test, you will need to stop eating anything from after dinner right through until you have your test.
On the day of your test: You will go into the hospital and change into a hospital gown. A cannula (thin tube) will be placed into a vein in your arm. This avoids having repeat needles and is used to administer medications. You will be given pain relief but will be awake during the procedure. The test takes around 4 hours, including recovery time afterwards.
For this test, blood samples need to be collected from the left and right inferior petrosal sinuses. To access these sites, a thin catheter is inserted into a vein in the groin area and passed through the veins until it reaches the right position – which is observed using x-ray imaging. Blood samples will be collected from around the sinuses as well as your arm to measure baseline ACTH.
Corticotropin releasing hormone (CRH) is then administered through the cannula in your arm. This should cause ACTH levels to increase. Blood samples will be collected for around 15 minutes to monitor changes in ACTH.
The catheter will then be removed, and your groin bandaged. You will remain in recovery for around 2 hours. After the test, you should limit strenuous physical activity for two days.
10. Vision test
Your doctor may organise to test your vision. This is because larger pituitary tumours can sometimes push on the nerves that connect the eye to the brain, called the optic nerve. This causes patchy or blurred vision, particularly at the far edges of your sight. Vision tests are most often conducted through eye specialists (an optometrist or ophthalmologist).
11. Bone mineral density (BMD) test
Your doctor may test your bone mineral density. This is because Cushing’s disease can increase the risk of osteoporosis (thinning and weakening of the bones, resulting in an increased risk of fracture). The best way to test bone mineral density is using a DEXA scan (Dual Energy X-ray Absorptiometry scan).
This is a fairly quick (10-30 minutes) and painless imaging procedure with less radiation exposure than a chest x-ray. It involves lying fully clothed on a platform while a scanner passes over you to take pictures of your hip, spine and, sometimes, forearm.
How is Cushing’s Disease treated?
Your doctor will tailor the treatment of your Cushing’s disease based on your symptoms and test results. The goals of treatment are to return cortisol to normal levels, reverse your symptoms and improve overall quality of life. Most often, this involves removing the tumour through surgery. However sometimes this isn’t possible and other treatments or medications can be used.
Surgery
The first line of treatment for Cushing’s disease is surgery to remove the pituitary tumour. The most common type of surgery is transsphenoidal surgery. This involves accessing the pituitary gland through the nasal passages, which minimises damage and scarring.
Transsphenoidal surgery is commonly performed by two surgeons: a neurosurgeon; and an ear, nose and throat (ENT) surgeon. The ENT surgeon uses an endoscope (a very thin fibre optic tube with a camera on the end) to navigate through one of your nostrils to the back of the nose where a small cut is made to access the pituitary gland. The ENT surgeon uses the endoscope to assist the neurosurgeon to see and remove the tumour. Larger tumours may need to be removed in smaller pieces. Once the tumour is removed a piece of tissue from the inside of your nose or some fat tissue is used to patch the hole at the back of the nose. This surgery leaves no visible scars.
The surgery takes about 2-3 hours and you will stay in hospital for 3-5 days. During your hospital stay your urine output is watched carefully and if your cortisol levels fall with removal of the tumour you will be prescribed some steroid medication. You will have regular blood tests while in hospital. After surgery, it is fairly common to have a mild headache, nasal congestion and reduced smell for 2-4 weeks.
You will have another blood test 4-6 weeks after surgery to check your cortisol and other hormones levels. Thereafter, your hormone levels will be checked periodically. An MRI scan will be done after 3-6 months. If symptoms reappear, blood tests and scanning will be repeated, and you may require repeat surgery at a later date or other treatments and/or medication.
In some patients, the tumour is entwined with the pituitary gland so that part or all of the pituitary gland has to be removed with the tumour. If this is the case, you will likely need long-term hormone replacement therapy.
After Surgery
It is not uncommon after a successful surgery, to feel worse while you recover and this can last a number of months. This is because your body needs to adjust to no longer having high cortisol levels, and both your pituitary gland and adrenal glands may take some time to resume normal function. You may experience headaches, aches and pains and extreme tiredness.
Your doctor will monitor your cortisol levels regularly over the first few months, with replacement steroid doses gradually reduced over time. This allows the recovery of your pituitary and adrenal gland function while balancing your body’s adjustment to lower cortisol levels.
Cortisol replacement therapy / steroid therapy
While you are taking cortisol replacement therapy, it is important to increase your medication during illness, surgery, trauma or stress. This is because your body needs more cortisol to cope with these conditions, and a natural rise would occur if your pituitary and adrenal glands were working normally.
Your doctor will discuss this with you and advise when and how to adjust your medications. This is important to avoid an adrenal crisis.
Increase the dose of glucocorticoid if you have:
- Illness with fever – double your dose for milder illnesses, and triple for more severe illnesses for 3 days or until well.
- Surgery or childbirth – You will require additional glucocorticoid doses. This should be planned ahead of time with your doctor.
- Severe trauma, such as a car accident or sports injury
- When you are experiencing high amounts of physical or emotional stress
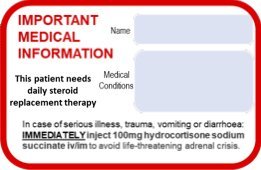
When diarrhoea or vomiting occurs, it is unlikely your medication will be absorbed properly, so medication will need to be given by injection (Solu-Cortef). If you are unable to administer emergency Solu-Cortef or your condition does not improve rapidly after use of the injection you should promptly present to your local emergency department.
Radiotherapy
Radiation of pituitary tumours is used to control tumour growth and hormone production and is offered when surgery is not possible or does not completely remove the pituitary tumour. Radiotherapy can also cause the tumour to shrink, although this can take months to years. While waiting for the radiotherapy to have its full effect, medication is often given to help control cortisol production.
Radiation is administered as an outpatient in a specialist centre. This therapy is commonly given using linear accelerators (high energy x-ray machines) which focus the beam on the pituitary tumour. Other methods of radiation may be available to you such as gamma knife radiotherapy. Sometimes with small tumours radiotherapy can be delivered at high dose in one session (often called radiosurgery).
Otherwise you will generally attend several treatment sessions, which reduces the chance of damaging other tissue. Your cortisol levels will be monitored after treatment, so that medications can be adjusted based on your needs.
Medication
Medications can be used to reduce high cortisol levels. These may be needed while waiting for surgery, following surgery if cortisol levels do not come down or while waiting for radiotherapy to take effect.
Several medications are available that act in different ways. These include medications that block the adrenal glands from releasing cortisol (orsilodrostat, ketoconazole, metyrapone and mitotane), medications that stop the pituitary gland from releasing ACTH (cabergoline and pasireotide) and medications that prevent cortisol from having an effect in the body (mifepristone).
Adjusting treatment during illness, surgery, trauma or stress
In people with adrenal insufficiency, cortisol levels do not automatically rise in response to illness, surgery, trauma or stress, as the adrenal glands cannot produce enough cortisol. This is why it is essential to increase glucocorticoid doses at these times to avoid an adrenal crisis.
An increase in the dose of glucocorticoid is needed if you have:
- Illness with fever – double for milder illness and triple for more severe illness for 3 days or until well.
- Surgery or childbirth – require additional glucocorticoid doses, and this should be planned ahead of time.
- Severe trauma (e.g. a car accident or sports injury)
- High amounts of stress
Your doctor will discuss this with you and advise when and how to adjust your medications. This sick day management plan can be downloaded and completed by your doctor. This provides a clear outline for how much medication to take when you are not well.
When diarrhoea or vomiting occurs, it is unlikely the medication is being absorbed properly. If these occur, the medication needs to be given by injection.
Injectable hydrocortisone (100mg; Solu-Cortef) can be given intramuscularly (into a muscle) or subcutaneously (under the skin) by patients or their family for times when oral medication is not enough or possible, such as vomiting, diarrhoea, other serious illness or if unconscious. Ask for training in this if it is not offered promptly after your diagnosis. Instructions about how to administer Solu-Cortef should also be carried, in case you are unconscious.
After Solu-Cortef is administered, you should still be transported to medical care (emergency department or hospital).
What is an adrenal crisis?
An adrenal crisis can occur when a person with cortisol deficiency or taking cortisol replacement therapy is exposed to severe physical or psychological stress, such as infection, illness, surgery or trauma. This is a medical emergency and requires an immediate injection of hydrocortisone (Solu-Cortef) to avoid becoming unconscious.
Symptoms of an adrenal crisis
The symptoms of an adrenal crisis include:
- Severe low blood pressure (shock)
- Altered level of consciousness and/or confusion
- Worsening of all symptoms of adrenal insufficiency and sometimes sudden pain in the back, stomach or legs
Treatment during an adrenal crisis
In cases of adrenal crisis, use the injectable hydrocortisone (Solu Cortef) BEFORE professional help (paramedics, doctors) arrives. This is very important even if going to hospital, as there can be delays in processing Emergency Department patients.
Injectable hydrocortisone (100mg; Solu-Cortef) can be given intramuscularly (into a muscle) or subcutaneously (under the skin) by patients or their family for times when oral medication is not enough or possible, such as vomiting, diarrhoea, other serious illness or if unconscious. Ask for training through your endocrinologist if it is not offered promptly after your diagnosis. Instructions about how to administer Solu-Cortef should also be carried, in case you are unconscious.
After Solu-Cortef is administered, you should still be transported to medical care (emergency
department or hospital).
How can I be prepared?
If you are taking cortisol replacement / steroid therapy, know your sick day management plan and wear an alert bracelet and carry a steroid card
Your doctor will go over your sick day management plan with you. This will include when and how to adjust your medication when you are not well. You can download and complete this sick day management plan with your doctor so you have a record. It is a good idea to take a photo of this on your phone, so that it can be with you at all times.
It is advisable to wear a medical alert bracelet with information, such as “give hydrocortisone” or “adrenal insufficiency – steroid dependent” to inform medical attendants that you need medication if you are too unwell to tell them in person. It is also useful to tell your friends and family about your need for extra medication when you are unwell.
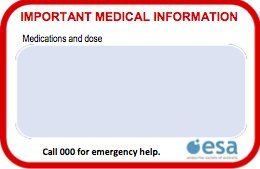
You should also carry emergency medical information with you, such as your medications and the name of your doctor.
A “Steroid card” for your wallet or purse is also recommended. This card can be used to record the details of your medical condition and medications for use in emergency situations.
The ESA credit-card sized steroid card is available for download here.
Your doctor can help you fill in the card. This can then be folded in half and laminated to fit easily in your wallet, purse or bag.
By carrying emergency medical information, others can help if an adrenal crisis occurs.
Have regular check-ups with your doctor
Cushing’s disease can be difficult to manage as symptoms and hormone levels can change over time.
This is why it is necessary to have regular check-ups with your doctor each year. Your doctor will make sure you are taking the right dose of medication to minimise your symptoms and control your hormone levels. They will also check your tumour has not returned, which occurs in around one quarter of all patients and can occur even many years following surgery.
Sometimes surgery and radiation can affect the ability of the pituitary gland to release other pituitary hormones. This is a condition called hypopituitarism and may require long-term use of different hormone replacement therapies, depending on which hormones are low or missing.
Regular check-ups with your doctor will allow them to monitor your hormone levels and adjust your medications to keep hormones in a healthy range.
FAQs about Cushing’s Disease
When to see your doctor
You should see your doctor (GP) if you have symptoms of Cushing’s disease.
Following diagnosis, regular check-ups with your doctor will help to monitor your condition, ensure your receive the right treatment, and adjust medications as required.
If you are having signs of an adrenal crisis, it is important to get medical help quickly, using emergency services (dialling 000) if needed.
Questions to ask your doctor
Seeing your doctor or having a medical problem can be stressful. It often takes time for information to sink in and it is very common to feel overwhelmed by what is happening.
Sometimes it is helpful to write down questions for your doctor before you go.
Some questions that might be relevant to you are:
- Do I have Cushing’s disease or Cushing’s syndrome?
- Do I need surgery for my Cushing’s disease?
- Do I need medications for my Cushing’s disease?
- Do I need to take hormone replacement medications?
- What are my choices for medication?
- How quickly should the medicine work?
- For how long do I need to take my medications?
- What should I expect with my symptoms?
- Does my medication have any side effects?
- Do I need to have an MRI?
- Do I need a bone mineral density scan?
- Do I keep taking my medication or hormone replacement if I get pregnant?
- Will I be able to breastfeed while taking medication or hormone replacements?
- Do I need another appointment?
Common terms and definitions
Adenoma – a non-cancerous tumour that occurs in glands
Adrenal – gland that sits above each kidney. It is divided into an outer layer (cortex) that makes corticosteroids and an inner layer (medulla) that makes adrenaline
Benign – a benign tumour is one that is not cancerous
Corticosteroid – type of steroid hormone made by the adrenal gland, and a term used to refer to related medications. Corticosteroids include glucocorticoids (e.g. cortisol), mineralocorticoids (e.g. aldosterone) and adrenal androgens (e.g. DHEA)
Glucocorticoid – the natural adrenal hormone cortisol and related medications such as hydrocortisone, cortisone acetate, prednisolone and dexamethasone
Hypopituitarism – a condition where the pituitary gland cannot produce enough pituitary hormones
Pituitary – small gland situated just underneath the brain that controls hormone production from a number of other glands such as the thyroid, adrenals, ovaries and testes
Tumour – an abnormal swelling or growth in the body. Can be benign or malignant (cancerous)
The content on this page has been medically reviewed by Professor Ann McCormack.
We are extremely grateful to Malini Raj from the Australian Pituitary Foundation for reviewing this information.